What is eosinophilic esophagitis (EoE)?
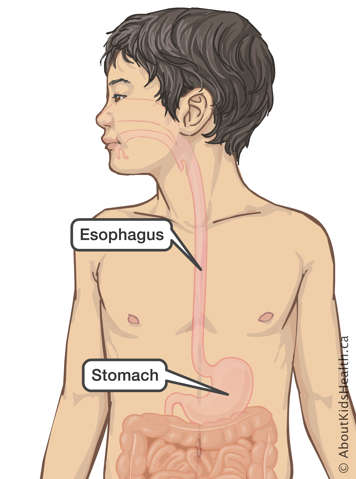
EoE is a chronic allergic/immune disorder that involves the esophagus, the tube that leads from the back of the throat into the stomach. It is called “eosinophilic” esophagitis because eosinophils, a type of white blood cells, are the cause of the inflammation and swelling in the esophagus. This inflammation and swelling can make it difficult for your child to swallow food and, sometimes, medications or supplements. Food, medications and supplements may also even get stuck in the esophagus.
EoE can affect people of any age, gender and ethnic background. It is more likely to occur in those who have allergies (such as asthma), food and seasonal allergies and eczema. EoE seems to affect males more often than females (3 to 1) and can run in families. It is thought to occur in about one in 10,000 children and across all ethnic groups.
Symptoms of EoE
Symptoms of EoE may be different between people and ages.
Common EoE symptoms by age
| Age group | Signs and symptoms |
|---|---|
| Infant and child |
|
| Adolescent/teen |
|
| Young adult/adult |
|
A person with EoE may not experience symptoms every time they eat, and they may only experience symptoms when eating certain foods.
Sometimes, food can become firmly stuck in the esophagus. This is called a food impaction. Food impactions can be stressful and are more likely to occur when eating dry foods, like crackers, or foods that require a lot of chewing, like chicken or hot dogs. If the food does not pass with swallowing, drinking liquids or by coughing it up, you should take your child to the emergency room where an endoscopy may be needed to take the food out of the esophagus.
What causes eosinophilic esophagitis?
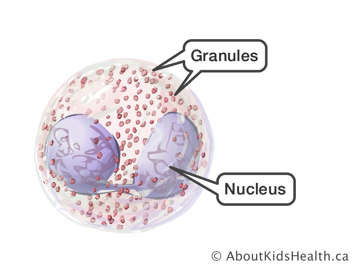
Normally, there are no eosinophils in the esophagus. EoE happens when many eosinophils gather in the lining of the esophagus and release granules that cause inflammation. Eosinophils are a type of white blood cells that are made in the bone marrow. They are an important part of the immune system because they help to fight off certain types of infections. When there are too many eosinophils in one part of the body, they can cause inflammation. These cells also play a role in the mechanisms that cause allergies and asthma.
The cause of EoE is not yet known, but several triggers likely play a role; and each person’s triggers can be different. Food allergies, sensitivities to food or environmental allergies may trigger eosinophils to gather in the lining of the esophagus. The most common foods that have been found to cause an EoE reaction are cow’s milk, wheat, soy, egg, peanut and tree nuts, and fish and seafood. Most people with EoE usually only react to one or two of these foods. People with environmental allergies, like a pollen or grass allergy, often experience EoE symptoms more often during “allergy season” (usually Spring and Fall).
People with EoE often have other allergic conditions such as asthma, eczema, seasonal runny nose and sinus problems.
Complications of EoE
Over time, the inflammation triggered by eosinophils can cause fibers deep in the esophagus to become tough, making the esophagus stiffer and less stretchy. This is called fibrosis. Fibrosis may make it difficult for your child to swallow foods and/or cause food impactions (food to get stuck in the esophagus). If untreated, long-term fibrosis can lead to strictures (permanent narrowing of the esophagus).
Diagnosis of EoE
A visit to a paediatric gastroenterologist will help with both the diagnosis of EoE and the creation of a treatment plan for your child if EoE is confirmed.
If your child’s symptoms are suggestive of EoE, several tests may be ordered. Often, imaging tests called esophagus-stomach-duodenum (ESD) and esophagus-stomach-small-bowel (ESSB) tests will be ordered to look for any narrowing of the esophagus. These tests use X-rays and a contrast medium to look at parts of the digestive system.
An upper endoscopy will also be organized. During the endoscopy, the gastroenterologist will be able to see what the esophagus looks like from the inside and take samples of the lining of the esophagus, called biopsies. These biopsies are sent to a pathologist who will look under a microscope and count the number of eosinophils in the tissue samples. An upper endoscopy is performed to diagnose EoE, but also to follow and assess your child’s response to their treatment plan.
Your child may also be sent to see an allergist. If your child is diagnosed with an allergy, the allergist will determine if your child requires epinephrine (an EpiPen) and provide guidance on how to use it.
Treatment for EoE
The main goal of treatment for EoE is to clear out the eosinophils in the esophagus. Over time, removing eosinophils from the esophagus lining helps decrease swelling and can even eliminate fibrosis.
You and your child will work with your child’s health-care team to decide which treatment approach is best. Your child’s team may include paediatric gastroenterologists, dietitians and nurses with knowledge of EoE. An allergist may also be involved in your child’s care.
There are several treatment choices for EoE. One type of treatment is not necessarily better than another. The two main types of treatment include medication and diet therapy. Some people with EoE respond well to one type of therapy, and some require both. Some people with EoE may also need to have a dilatation of the esophagus, which is a procedure that helps open up any narrowing.
Medication
Two groups of medications are commonly used to treat EoE: topical steroids and proton pump inhibitors (PPIs).
Topical steroids
Your child may be prescribed a mild topical steroid medication such as budesonide or fluticasone. Topical steroids work at the surface of the esophagus lining to reduce inflammation. The purpose of this medication is to reduce the number of eosinophils in the esophagus and help your child with any symptoms of EoE, like difficulty swallowing. The steroids used are the same as those used in the inhalers used to treat asthma; but instead of inhaling the medication, it is swallowed.
Budesonide is a liquid that is mixed with a thickener and ingested so it coats and sticks to the esophagus on the way down. Budesonide is also available as a dissolving tablet. Fluticasone is a spray that your child sprays into their mouth. After waiting for a few seconds, it is swallowed with your child’s saliva. If your child takes the medication as directed, their symptoms should improve within days or weeks.
Proton pump inhibitors (PPIs)
Other frequently prescribed medication for EoE are PPIs such as omeprazole, lansoprazole or rabeprazole. The purpose of this medication is also to reduce the inflammation and number of eosinophils in the esophagus. PPIs reduce the production of stomach acid and can also help with symptoms of acid reflux.
Diet therapy
Dietary changes can also be used to treat EoE. This is called diet therapy. Some foods can trigger eosinophil production and inflammation. By removing these foods from the diet, symptoms of EoE and inflammation can be reduced.
Diet changes are guided by your child’s health-care team. The foods that are most commonly removed in order to treat EoE are cow’s milk and wheat (both often removed at the same time). However, your child’s health-care team will provide diet therapy advice that is specific to your child.
Sometimes, your child’s health-care team will suggest removing many foods from your child's diet all at once. This is called an EoE elimination diet. As part of managing your child’s EoE with diet therapy, the health-care team will make sure that your child gets enough energy (calories) and nutrients to grow and develop.
There are a few different ways to approach EoE elimination diets:
- Remove foods identified by an allergist.
- Remove foods identified by an allergist and/or other foods known to worsen symptoms in EoE. This can include two, four, six or more foods. The most common foods known to trigger inflammation in EoE are cow’s milk, wheat, soy, eggs, peanuts and tree nuts, and fish and seafood.
- Remove all foods from your child’s diet. This type of elimination diet is the strictest and is sometimes called elemental therapy. Your child is prescribed special liquid nutrition for four to eight weeks. During the time your child is on strict elimination therapy, they are not allowed to eat any other foods. After four to eight weeks, foods are slowly reintroduced into their diet while monitoring for symptoms of EoE. You should not attempt to try elimination therapy without the advice and supervision of your child’s health-care team.
Your child’s health-care team may recommend a combination of medication and diet therapy. How well your child responds to therapies will be assessed by the reduction of symptoms and/or eosinophils seen in an esophagus biopsy.
Living with eosinophilic esophagitis
Beyond the goal of reducing inflammation and EoE symptoms, it is important to help support your child’s growth, development and quality of life (like their participation in everyday activities). Coping with a chronic condition like EoE may involve taking medications every day or following dietary restrictions—even when your child feels well—and sticking to these routines can be hard for anyone, especially children or teens. It can also be stressful for parents and caregivers. If you or your child are having trouble dealing with the treatment of EoE, remember:
- Keep the lines of communication open between you, your child and their health-care team.
- Be sure to let your child know that it is normal to feel sad or anxious.
- Assure your child that taking their medications every day and/or following diet therapy will help them to lead a healthy life.
- Let your child know it is important to talk about their feelings with a parent or a doctor.
It is important that adolescents with EoE have an active role in understanding their condition and managing their clinic visits and therapy plans. As your child gets ready to move into adult care (after the age of 18) their team will assess their EoE status and follow-up care.
Follow-up care
In general, your child will be followed regularly by a paediatric gastroenterologist and, in some cases, by a team that may include a dietitian, nurse and allergist.
EoE is a chronic condition that requires ongoing observation and management. It is not currently known how long EoE has to be present before strictures (narrowing of the esophagus) form. There is little data that suggests EoE causes cancer of the esophagus, and EoE does not appear to affect life expectancy. What is known about the natural history and course of EoE continues to evolve, so close monitoring and long-term follow-up of your child is advised.