How does the heart beat?
The heartbeat is controlled by electricity. Special cells called pacemakers release bursts of electrical energy that travel through the heart muscle, causing it to contract. When the muscle contracts, blood is pumped through the heart.
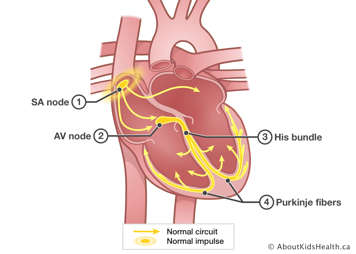
To learn more about the heart's electrical system and the normal heartbeat, please see How the Body Works: Electrocardiogram (ECG).
What is an arrhythmia?
An arrhythmia (also called dysrhythmia) refers to what is usually an irregular heartbeat. The heart rate can be fast, slow or irregular, taking into consideration age and activity. For example, a newborn's heart beats much faster than a five-year-old child's heart.
A fast heart rate is called tachycardia. A slow heart rate is called bradycardia.
Some irregular heartbeats are normal:
- Sinus arrhythmia is the normal variation in heart rate that accompanies breathing in and out.
- Sinus tachycardia is the normal increase in the heart rate that occurs in healthy people when they are excited, exercising or have a fever.
An arrhythmia can be short-lived (acute) and resolve on its own, or long-lasting (chronic) requiring treatment.
Arrhythmias can occur at any age and may or may not cause symptoms.
Different types of arrhythmias, and some syndromes that can cause arrhythmias, are described below.
What is tachycardia?
Tachycardia is a fast heart rate. With tachycardia, the resting heart rate for a newborn can increase to over 160 beats per minute. This can last for seconds, minutes or even hours, depending on how serious it is. Symptoms include feeling dizzy, weak and generally uncomfortable.
It is important to know that it is unusual for tachycardia to cause the heart to stop all of a sudden, and it usually does not last long enough to cause serious damage.
There are two basic types of tachycardia:
- ventricular tachycardia, which involves only the ventricles
- supraventricular tachycardia (SVT), which involves both the atria and the ventricles; this is the most common type in children
For more information, please read Fast heart rate (tachycardia).
How is tachycardia treated?
Treatment depends on what is causing the tachycardia. Some SVTs can be stopped with certain techniques called vasovagal manoeuvres, including:
- blowing on your thumb like it's a horn
- blowing through a straw with your hand on the end to plug it
- putting ice or cold water on the face for a few seconds
Other tachycardias can be helped with medication. Drugs can help prevent the episodes from starting, decrease the heart rate during the episode or shorten how long the episode lasts.
Radiofrequency catheter ablation (RFCA) is another option. This approach delivers electricity to the heart to permanently interrupt the abnormal electrical pathway. One of the newer approaches is cryoablation, which involves the use of freezing.
What is bradycardia?
Bradycardia is a slow heart rate. It is less common than tachycardia.
Bradycardia is usually caused by damage to the sinus node, which is the heart's natural pacemaker. This can occur during surgery or from abnormalities of the sinus node (sick sinus syndrome). It can also be caused by heart block.
When bradycardia is detected very soon after birth, it is sometimes caused by complete heart block, although it can also develop later in life (acquired heart block).
How is bradycardia treated?
In some cases, children may need to have surgery to implant a permanent pacemaker. In other cases, the condition is not serious.
What are premature heartbeats?
Premature heartbeats, or extra beats, usually cause irregular heart rhythms. These can start in the atria (premature atrial contraction or PAC) or in the ventricles (premature ventricular contraction or PVC).
This type of arrhythmia feels like your heart has "skipped a beat." What actually happens is a beat comes earlier than expected, then there is a pause, and then the next beat is very strong.
Premature heartbeats are often completely normal. Many people have them at one time or another. However, in some cases they may indicate disease or damage in the heart.
What is sick sinus syndrome?
The sinus node (also called the sinoatrial node) is the heart's natural pacemaker. When the sinus node does not work properly, it is called sick sinus syndrome. Children with this syndrome experience tachycardia and bradycardia.
Treatment may involve medication and/or an artificial pacemaker.
What is heart block?
Heart block means that the electrical signal that causes the heart to beat cannot move from the upper chambers of the heart (atria) to the lower chambers (ventricles). When this happens, another signal takes over in the lower chambers, but at a slower rate.
The most serious form of this condition is complete heart block. This heart rhythm abnormality can occur before birth (congenital heart block) or happen as a result of disease or injury (acquired heart block). Complete heart block is also known as third-degree heart block.
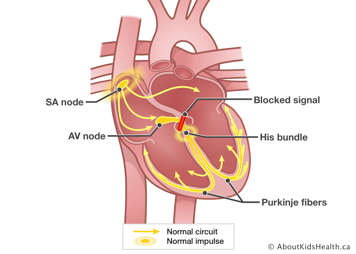
Congenital heart block is more common in children born to mothers with systemic lupus erythematosus (SLE) or related conditions. Exactly what causes heart block in these children is unknown. It is thought that mothers with this disease pass on the SLE antibodies to their babies. Antibodies are proteins that help protect against infection.
How is heart block treated?
When the heart's "pacemaker" cannot do its job properly, surgery to implant an artificial pacemaker may be done. Without treatment, the heart beats so slowly that it cannot get enough blood to the vital organs of the body.
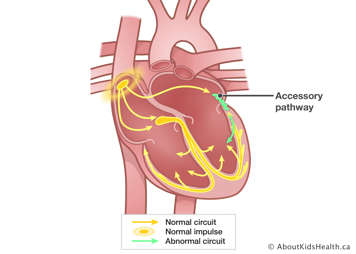
What is Wolff-Parkinson-White Syndrome (WPW)?
In WPW syndrome, an abnormal pathway that conducts electrical signals causes the signal to get to the ventricles too quickly. This condition may or may not have symptoms. It may be connected with supraventricular tachycardia. Occasionally, dangerous rhythms can be seen in patients with WPW.
How is WPW treated?
WPW can sometimes be successfully controlled with medication, but sometimes radiofrequency catheter ablation (RFCA) is needed.
What is long QT syndrome?
This syndrome involves electrical instability in the heart. The irregularity in the electrical conduction can cause ventricular tachycardia.
Long QT syndrome is not common and usually has no symptoms. Often, the first sign may be fainting under stress or during intense exercising.
In rare cases, long QT syndrome is associated with congenital deafness. It usually runs in families.
How is long QT syndrome treated?
In most cases, treatment is needed. Treatment usually involves the use of drugs called beta blockers, which can slow down the heart's reaction to stress. Treatment can also involve the use of pacemakers or implantable cardiac defibrillators.
What causes arrhythmias?
Arrhythmias can develop on their own (primary arrhythmia) or because of another condition, typically after heart surgery (secondary arrhythmia).
Some types of arrhythmia may have a genetic component. If someone in your family had an arrhythmia, it may be more likely that your child might too.
Arrhythmias can occur in structurally healthy hearts, but sometimes arrhythmias are a symptom of a heart abnormality.
Sometimes arrhythmias can be caused by an external factor, like a drug a child is taking or a fever.
How is an arrhythmia diagnosed?
You or your child may not notice anything unusual about their heart rhythm. Arrhythmias may be discovered during a usual check-up. The doctor may ask you questions like:
- Is your child aware of unusual heartbeats?
- Are unusual heartbeats brought on by anything in particular?
- If the heart rate is fast, how fast is it?
- Has your child shown any symptoms, like feeling weak or dizzy?
- Has your child ever fainted?
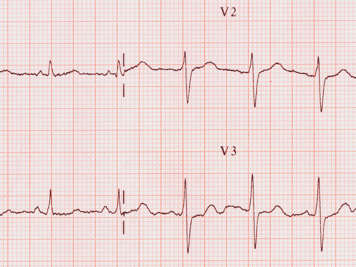
Arrhythmias are identified through electrocardiograms. These tests show the electrical activity in the atria (upper chambers) and the ventricles (lower chambers) of the heart. Doctors examine the heart rate activity, how often these electrical signals occur, and how regularly the heart beats to determine if a child has an arrhythmia.
A test called a Holter monitor may be done. This is a recording of an electrocardiogram reading for a 24-hour period. Because arrhythmias tend to happen only once in a while, it is important to monitor the child for a good amount of time.
For more information, please read Holter Monitors.
Fetal arrhythmias can also be identified when the baby is still in the womb. To manage this situation, the mother is generally given anti-arrhythmic drugs. Intermittent fetal tachycardias can pose a threat to the baby, possibly before or after birth, and the arrhythmias tend to recur in infancy.