Everything we contact in daily life potentially contains organisms which can cause infection. These include:
- bacteria, which are microscopic organisms that invade tissues and grow very quickly. They cause infections anywhere in the body.
- fungi, which are primitive organisms that we encounter everywhere, such as bread mold. Some harmless forms reside inside our bodies.
- viruses, which are parasites that are smaller than bacteria. They need another host, such as human cells, to survive and grow.
These daily sources of infection are not a major issue for a healthy person. Our immune system protects us from becoming infected.
Why is your child prone to infections?
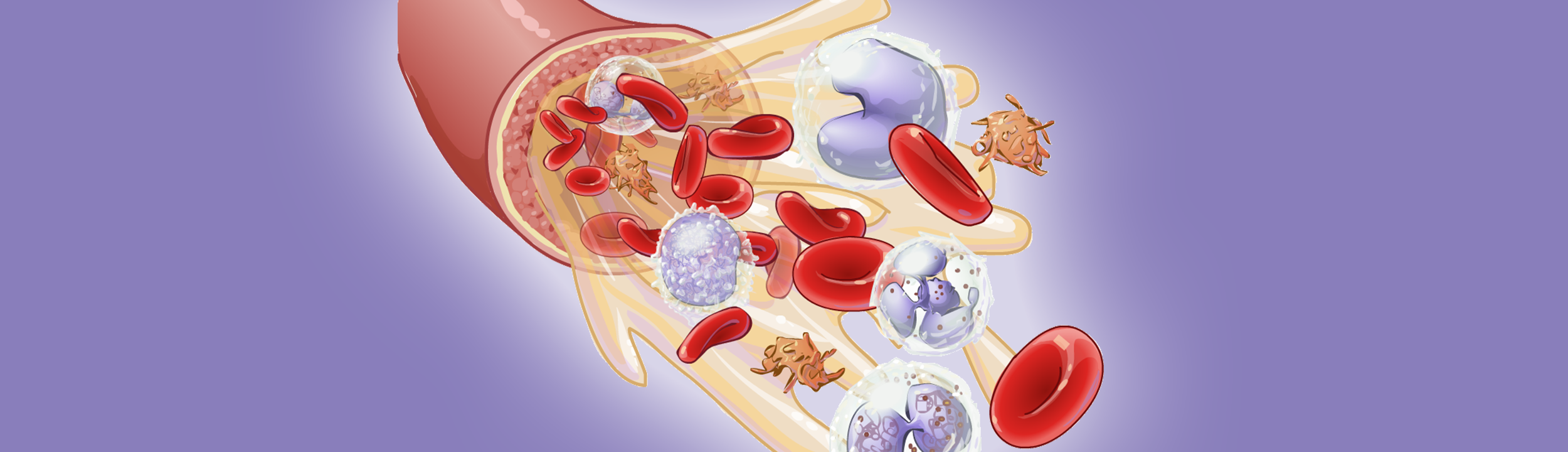
The high-dose chemotherapy or radiation your child receives before the transplant destroys both diseased and healthy cells. This helps make room for new, bone marrow cells. But the chemotherapy weakens your child’s immune system by destroying white blood cells. Having too few white blood cells is called neutropenia, in which unique proteins called antibodies which help destroy bacteria and viruses become limited. Until the transplanted marrow stem cells grow and produce new white cells, your child is extremely vulnerable to infection.
What are the symptoms?
It is very common for blood and marrow transplant patients to have fevers while in the hospital. Infection is often the cause of the fever. However, your child may also develop a fever because of chemotherapy, radiation or blood transfusions.
How will your child’s fever be checked for infection?
At the first sign of fever, several tests will be done to help the doctor find out the cause. The nurse will:
- draw blood from your child’s arm and from the central venous line (CVL)
- take a sample of your child’s urine to check for any signs of infection
- take a chest x-ray
- check your child’s temperature, which may be done through the mouth. On rare occasions, the nurse will take a rectal temperature. This is not done at home and should only be done by a health-care practitioner.
How are infections prevented?
To decrease the risk of your child developing an infection, they will be given some medicines prior to the transplant.
Fluconazole
To prevent fungal infections from developing, the doctor will give your child an anti-fungal medicine called fluconazole. This is given through your child’s mouth or intravenously (IV) until your child’s neutrophils counts improve.
Septra
Septra is an antibiotic that is used before your child’s transplant. After new white blood cells begin to grow in your child’s marrow, the doctor will give your child Septra or similar antibiotics called, called Dapsone or Pentamidine. These drugs will prevent a specific lung infection, caused by a common fungus named Pneumocystis jiroveci. It will be given by mouth for six months to a year after the transplant.
How is the infection treated?
To help lower your child’s fever, the nurse will give them acetaminophen, or Tylenol®.
To treat the fever, your child will be given several other medicines.
Antibiotics
Antibiotics are strong medicines that treat infections caused by bacteria. After the transplant, if your child’s temperature is about 38.0˚C the doctor will give large doses of antibiotics during the first few weeks. Your child must bathe or shower every day to wash away any bacteria on their skin. To avoid cuts where bacteria, fungi and viruses might enter, you child should use a soft toothbrush while cleaning their gums and teeth.
There are many different types of antibiotics. The doctors will choose the best one to fight your child's infection.
Amphotericin B
Although less common, some children may develop fungal infections. Amphotericin B is the drug most commonly used to treat a fungal infection.
Your child may develop chills the first time they take Amphotericin B. Your child’s nurse can treat the chills with medicines like Benadryl or Demerol. The nurse will also give your child other medicines to prevent the chills from occurring again.
Ganciclovir and foscarnet
Ganciclovir and foscarnet treat serious infections caused by a virus called the cytomegalovirus (CMV). CMV can infect the liver, colon, eyes or lungs. It is one of the most common viruses that can cause severe infection during your child’s transplant. Both your child and the donor are tested for CMV before the transplant. If your child or the donor test positive for CMV, the doctor will give your child ganciclovir or foscarnet.
Acyclovir
Acyclovir is a drug that prevents and treats cold sores, which is caused by the herpes simplex virus.
Gamimune (or immune globulin)
Gamimune is a concentrated preparation of antibodies, which help the body fight infections. Many transplant patients receive gamimune once a week until they are discharged.
G-CSF
G-CSF is a drug that stimulates the body to produce new neutrophils.
Not all children receive this drug. G-CSF is usually given to children:
- whose immune systems take a long time to recover after the transplant
- who develop unusually severe infections
The nurse may give G-CSF daily through your child's CVL until the amount of neutrophils in the blood increases to safe levels.
For more information, please see the page on Medicines and Side Effects.