What is systemic lupus erythematosus (lupus, SLE)?
Systemic lupus erythematosus is a disease that causes inflammation in many parts of the body. It is also called lupus or SLE.
Inflammation is the body's normal, protective response to injuries or infections. Inflammation is the work of the immune system and is usually an important part of the healing process in the body. Sometimes, the immune system can over-react and can cause inflammation by attacking healthy tissues within the body. This process can occur in many autoimmune diseases, including lupus. When it happens, the immune system mounts an inflammatory response in parts of the body that do not need healing in areas that you can see, or it can happen inside the body where it cannot be seen. The most common body parts involved in lupus include the:
- skin and hair
- kidneys
- brain
- joints and muscles
- heart
- lungs
- blood cells – red blood cells, white blood cells and platelets
Lupus is a chronic autoimmune disease. Chronic means that the disease can go on for many years. There will be times when the disease is active with symptoms (a flare), and there will be times when it is quiet (remission). The immune system normally helps to fight off infections caused by bacteria and viruses. In a person with an autoimmune disease, the immune system makes a mistake. Rather than fighting off germs, it attacks a person's own healthy cells. When this happens, the area becomes inflamed.
Symptoms of lupus
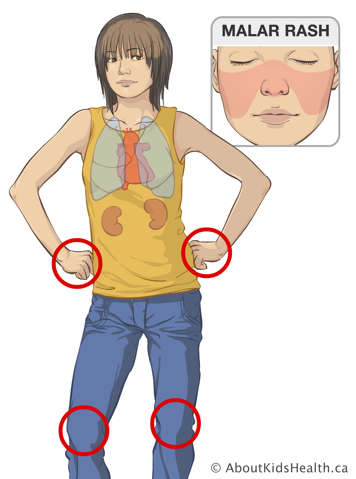
The signs and symptoms of lupus can vary greatly from person to person. They can be very mild or they can be much more severe. Specific signs and symptoms of lupus can be related to different parts of the body.
Skin and hair
A common symptom of lupus is a butterfly-shaped rash over the top of the nose and on the cheeks called a malar rash. In addition to the butterfly rash on the face, lupus can cause different types of rashes on almost any part of the body, including:
- pink or red rash on the body
- a scaly, raised, coin-shaped rash on any part of the body that leaves a scar when it heals (discoid rash)
- a rash that comes out when there is exposure to ultraviolet light from the sun or from a tanning booth (photosensitive rash)
- hair loss in the front, or patchy areas of hair loss all over
- sores in the mouth or nose that do not hurt
Kidneys
A child with lupus can have problems related to the kidneys, which cause the following symptoms:
- increased blood pressure
- swelling of the feet and around the eyes
- weight gain
- blood or protein in the urine during a check-up
Heart and lungs
Lupus can cause inflammation of the lining around the lungs (pleuritis) and/or heart (pericarditis), causing symptoms such as:
- chest pain
- shortness of breath
- difficulty breathing when lying down
- a feeling of tightness in the chest
Central nervous system (CNS)
Lupus can also cause symptoms related to the CNS (brain and spinal cord). These symptoms are all called CNS features and include:
- headaches
- memory or concentration difficulties
- mood swings
- hearing or seeing things that are not there (hallucinations)
- seizures
- low mood
- anxiety
Other symptoms of lupus
- pain, stiffness, warmth and swelling in the joints (arthritis)
- colour changes and/or sores on the fingers and toes (Raynaud's phenomenon)
- extreme tiredness (fatigue)
- fever
- weight loss and decreased appetite
- muscle pain and weakness
- easy bruising and bleeding (due to low platelet levels)
What causes lupus?
The cause of lupus is unknown. It is not a contagious disease and cannot be passed from one person to another. Nothing anyone did, or did not do, causes a child to develop lupus.
Lupus usually occurs between 13 and 45 years of age. It affects more females than males. It can, however, occur at a younger age.
The exact cause of lupus is a mystery. Individuals at any age and of any ethnicity may develop lupus. For most people, there is not one gene that causes lupus, but many genes working together may make it more likely for some people to develop lupus. We also know that the sun, certain medicines and some infections can make the disease worse. These things are known as 'triggers.'
How is lupus diagnosed?
Lupus may be difficult to diagnose because it can affect many different parts of the body. It has been called "the disease of a thousand faces." To make the diagnosis, your child or teen's health-care provider will:
- take a full history of all the symptoms
- do a physical examination
- collect blood and urine samples
They may order other tests to check specific areas of the body if they suspect a problem.
Treating lupus
Your child or teen may need to stay in the hospital while the lupus is brought under control. The treatments are aimed at controlling the inflammation in the body and making your child or teen feel better.
Lupus is treated with medicines that control inflammation and that help to prevent the immune system from attacking healthy cells. Other medicines may be needed if lupus has caused damage to specific body parts.
Some of the drugs most commonly used are:
- Hydroxychloroquine (Plaquenil): This oral medication treats the rash and joint pain of lupus and is very important in helping to prevent new symptoms and flares of lupus.
- Prednisone: This is a type of steroid that is given orally to control inflammation. Intravenous steroids are also sometimes given.
- Non-steroidal anti-inflammatory drugs (NSAIDs): NSAIDs, such as naproxen or ibuprofen, help control inflammation.
- Immunosuppressive medicines: These help settle down the immune system. These include methotrexate, azathioprine, mycophenolate mofetil (MMF), tacrolimus, cyclophosphamide and leflunomide.
- Biologic medicines: These are newer medicines that can target molecules in the immune system. These include rituximab and belimumab. There are other biologic medicines that are being studied in children and teens with lupus, including anifrolumab and obinutuzumab.
Many children with lupus will need to take other medicines to help control their blood pressure if they have kidney disease. Sometimes, stomach-protecting drugs may be needed to prevent side effects of medications. The health-care team may also recommend supplementing with calcium and vitamin D.
Most drugs have some side effects, which are not part of the treatment. When your child is prescribed a medicine, the health-care team will let you know how it works, what side effects can occur and what that might mean to your child. Using a pill box can make taking the medicines easier and less confusing.
Living with lupus
Lupus may affect your child's usual activities
Your child may experience fatigue and pain, making it hard to do normal activities. At times, your child may not feel like going out with friends or going to school. The goal is to help make them feel better and be able to get back to doing all of these things.
Lupus may affect your child's school attendance and performance
Your child may have to miss a lot of school due to illness, being hospitalized or going to medical appointments. They may also have trouble keeping up with all the activities and schoolwork. Let the school know about your child's illness. They may be able to offer suggestions on making things easier and decreasing stress. Your child’s health-care provider may be able to write a letter or contact the school if this is needed.
Lupus can affect the whole family
When a child is diagnosed with a disease, it can be a very scary time for everyone. Sometimes the disease seems to get better and at other times it suddenly seems to get worse. This can be very stressful for the whole family. Other children in the family may resent the extra attention that the sick child needs. There may be feelings of guilt and fear of the unknown. Your child may feel sad and wonder "why me?"
If these issues arise in your family, you can speak with a counsellor or your child's health-care team for support and guidance. They will be able to help you through these hard times and give you ideas to make things a little easier for everyone.
When your child is newly diagnosed with lupus or having a flare up of the disease, they may have some difficulty doing the same things as before. The health-care team can help you to adapt to situations and to set realistic goals for you, your child and your family.
Try to keep your child doing the same things that they did before the disease, whenever possible. Daily routines are important to children and often quite comforting. If routines can change as little as possible, this will help your child feel better about how the disease has affected them. Routines can include school, home, chores, exercise and extracurricular activities, and spending time with friends and family. If you are unsure of what your child can do, ask one of the health-care team members.
Follow-up care
Your child will be seen in the lupus clinic for follow-up care. In the beginning, it may seem that you are going to many appointments. As your child's condition improves, the appointments will be less frequent. Your child's lupus health-care team includes a nurse and doctors from Rheumatology and Nephrology (kidney doctors). The team may also include:
- social worker
- dietitian
- physiotherapist
- teen specialist
- psychologist
- pharmacist
At every clinic visit, your child will have bloodwork and be asked to give a urine sample. This is done to help the health-care team see how active your child's disease is and to see how well the medicines are working. You and your child or teen are encouraged to keep track of their medications – the names, what they do, and when and how to take them.
After you have met with the lupus team, you will know more about how to care for your child and the plan for future clinic visits.