At the end of this chapter, you will be able to:
- identify types and parts of your child’s tracheostomy tube
- review how tracheostomy tubes function
- identify components of a tracheostomy emergency kit
What is a tracheotomy?
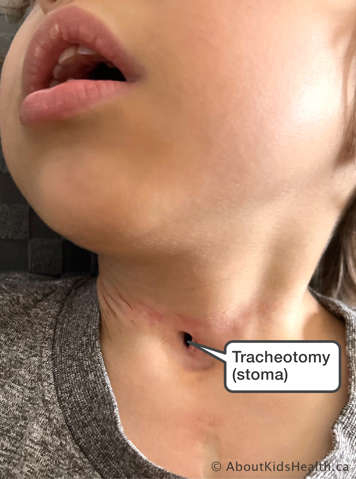
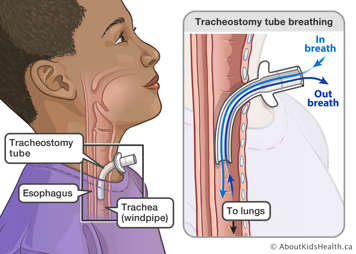
A tracheotomy is a hole through the skin in the front of the neck and into the trachea. The hole is created during surgery. The opening in the neck is called a stoma.
What is a tracheostomy tube?

A tracheostomy tube is inserted into the trachea (windpipe) in the neck and keeps the stoma open. It is held in place with ties that go around the neck. The opening of the tracheostomy tube can be covered with prescribed tracheostomy adjuncts. You will learn about these in upcoming sections.
You may hear both words tracheotomy and tracheostomy used in the community. While they mean different things to health-care providers, in common speech, it doesn’t matter all that much.
Why does my child need a tracheostomy tube?

Your child needs a tracheostomy tube to help with their breathing. The tracheostomy tube can:
- bypass a block in the upper airway
- help manage your child's secretions
- keep the airway safe if your child’s cough or gag reflex is not working properly
- allow your child to receive long-term ventilation at home
What changes can I expect in my child once they have a tracheostomy tube?
Physical appearance
A tracheostomy tube can be seen on the front of the neck. It may take some time for you and others to get used to seeing your child's neck look different.
Humidification (adding moisture to the air your child breathes)
When your child breathes through a tracheostomy tube, the air goes right into their lungs rather than through the nose and mouth. As a result, the air is not warmed or moistened. However, your health-care team will show you which humidification systems to use to moisten the air your child breathes.
Quality of air reaching lungs
Because the air your child breathes bypasses the nose and mouth, it can still contain tiny amounts of dirt, dust and germs that would normally be filtered out. As a result, your child may have more frequent lung infections once they have a tracheostomy tube.
Secretions
Your child's cough is the best way to clear any dirt, dust or germs that your child breathes into their lungs. With a tracheostomy tube in place, your child's cough will not be as strong. The tube itself can also interfere with clearance of secretions (mucus). This may lead to a build-up of secretions, which would normally be swallowed or coughed out. Your child may need help to clear these secretions through suctioning.
Eating and drinking
If your child was able to eat or drink by mouth before the tracheostomy tube was inserted, it may take some time for them to be able to eat with a tracheostomy tube in place. The occupational therapist, a feeding specialist and/or a speech-language pathologist will work with your child to assess their swallowing safety.
Speaking
A tracheostomy interferes with a child’s ability to produce voice as the exhaled air does not pass between the vocal folds/through the voice box. The exhaled air goes out of the tracheostomy tube opening and is not directed to the upper airway. However, communication devices and techniques are available for redirecting airflow to the upper airway.
Constipation
A tracheostomy tube may impair a child’s ability to strain when having a bowel movement. This can lead to constipation. Your child may need a good bowel regimen to resolve this. Your child’s doctor or dietitian can offer more advice.
Monitoring requirements
It is recommended that a child with a tracheostomy is always monitored by a trained caregiver. An oximeter is also highly recommended for monitoring. Your child’s health-care provider will prescribe an oximeter and explain when it should be used on your child.