At the end of this chapter, you will be able to:
- understand when you need to perform deep suctioning
- demonstrate how to perform deep suctioning
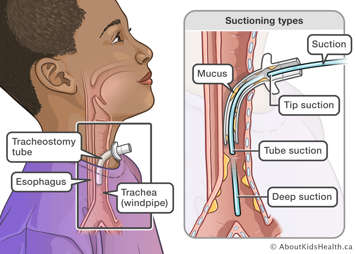
Deep suctioning is done to clear secretions (mucus) from beyond the level of the tracheostomy tube if a child is unable to clear it on their own through coughing or if the child is in respiratory distress and tube suctioning does not resolve the secretion issues.
Precautions
Deep suctioning is done in urgent situations. Frequent deep suctioning can injure the airway. If you have to deep suction your child more often, it should be brought to the attention of their health-care provider.
-

Gather your equipment and supplies, including oxygen, if available.
-

Make sure the oximeter is on and provides an accurate reading.
-

Make sure the suction machine is at the correct setting.
-

Wash your hands well. Deep suctioning is done in urgent situations so to save time, you may choose to use hand sanitizer instead of soap and water. Parents and caregivers do not need to wear gloves, although you may choose to do so if you have them. If you have a home nurse visiting, they will bring their own gloves and wear them.
-

Fill a clean container with sterile, distilled water or saline.
-

Make sure your child is in a comfortable position (lying or sitting).
Put on clean gloves, if using (see above).
-

Verify catheter size. Next, open the catheter by pushing the base through the paper packaging.
-

Attach the suction tubing to the correct size suction catheter.
-

Withdraw the catheter from the package slowly just before use. Hold it four to six inches from the end.
Do not touch the end of the catheter that goes into the tracheostomy tube. Keep the catheter inside the packaging until you use it.
Remove any ventilator connector, tracheostomy mask, Airvo tracheostomy connector, tracheostomy cap, heat and moisture exchanger (HME) or speaking valve from the tracheostomy tube. If necessary, manually ventilate the child with the manual resuscitation bag.
-

Gently insert the suction catheter into tracheotomy tube with your thumb off the suction control port. If needed, stabilize the tube. Controlling the suction port with your non-dominant hand and suctioning with your dominant hand is often helpful.
-

Once you meet resistance or your child starts to cough, pull the suction catheter back a small amount and then apply suction by holding your thumb over the suction control port.
-



Slowly remove the suction catheter to remove mucus (10 seconds max).
-

Apply suction and watch the thumb port region to assess the secretions obtained.
Take note of the quality (colour and consistency) of secretions and the quantity of secretions.
-

Clear the suction catheter if needed by dipping it in the sterile water or saline and suctioning.
Give your child a break of at least 30 seconds before repeating deep suctioning.
-

Assess and tend to your child’s respiratory status and oxygen needs after each suction pass. Give your child some manual breaths using the manual resuscitation bag if needed. In the event of oxygen desaturation, use oxygen as prescribed by your child’s health-care team.
When done, replace the tracheostomy adjunct your child uses: ventilator connector, tracheostomy mask, Airvo tracheostomy connector, tracheostomy cap, heat and moisture exchanger (HME) or speaking valve.
Once you are finished, suction up sterile water or saline in the catheter (called flushing) to rinse the suction tubing. Discard the catheter. Discard water.
Turn off the suction unit.
Empty and clean the suction drainage bottles and containers, if needed.
Wash hands well.
Prepare the suction equipment and supplies for the next use.
Precautions
Only perform deep suctioning if your child continues to have difficulty breathing after tube suctioning.