Managing diabetes is a little like performing a complicated juggling act. Sometimes the ball drops. No matter how hard you try, it is difficult to keep the
blood glucose (sugar) level in target range all of the time. Sometimes it will be high, other times low. Often there is no way of explaining the results.
What is "low blood sugar" (hypoglycemia)?
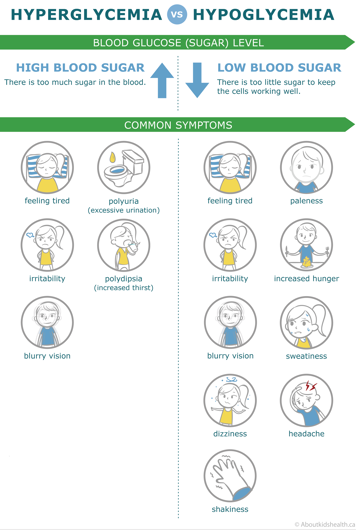
A "low blood sugar", or hypoglycemia, is a blood sugar level lower than 4.0 mmol/L; however, some people experience mild symptoms of hypoglycemia at blood sugar levels slightly higher than this.
In people without diabetes, the pancreas automatically stops producing insulin whenever blood sugar readings are at a normal level. But in patients with diabetes, injected insulin continues to push sugar into cells until there is virtually no more sugar in the bloodstream. The excess insulin in the bloodstream leads to hypoglycemia.
Most people with diabetes experience a low blood sugar from time to time. The warning signs let people with diabetes know that the body needs sugar quickly. Many, but not all, people with diabetes are able to detect the warning signs.
Mild to moderate symptoms (warning signs)
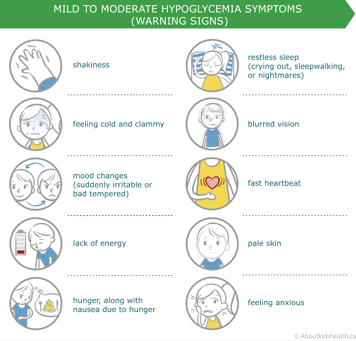
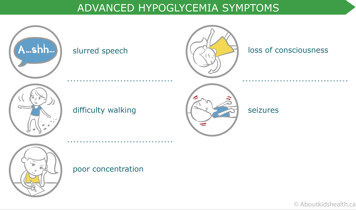
As blood sugar levels continue to drop, more advanced symptoms may begin to develop. Severe hypoglycemic events are less common and may be more difficult to treat.
Advanced symptoms
Important things to consider about hypoglycemic events
- They can happen quickly.
- They can occur day or night.
- Symptoms vary, but each child usually exhibit one or two tell-tale signs you will learn to recognize.
- Hypoglycemia can be difficult to detect in infants or very young children; good indicators are crying, irritability, pale skin, along with a “floppiness” of the head.
Treatment of mild low blood sugar
Treatment of "low blood sugar" (hypoglycemia) needs to occur quickly, regardless of how mild the symptoms are. It is important to always have a source of fast-acting sugar (sugar that will quickly raise blood sugar level) available, such as juice or dextrose tablets.
In the event of mild hypoglycemia, follow these steps:
- Check your child’s blood sugar level to confirm that it is low.
- For children under 6 years of age, a blood sugar level below 6.0 mmol/L with symptoms is enough for treatment.
- For children aged 6 years and older, a blood sugar level less than 4.0 mmol/L with symptoms is enough for treatment.
- Depending on your child’s weight, 5 to 15 grams of fast-acting sugar is all it takes. Please see the tables below:
| Less than 15 kg (33 lbs) | |
|---|---|
| Amount of carbohydrate required | 5 g |
| Fast-acting sugars and their carbohydrate content (g) |
Sugar: 1–1½ tsp (4–6 g) add to ¼ cup water Fruit Juice: 1½ oz (5 g) Chocolate milk: ¼ cup (7 g) White milk: ½ cup (6 g) Regular pop: ¼ cup (7 g) Jam/jelly: 1–1½ tsp (4–6 g) |
| 15-30 kg (33-66 lbs) | |
|---|---|
| Amount of carbohydrate required | 10 g |
| Fast-acting sugars and their carbohydrate content (g) |
Dextrose tablets: 2-3 (8–12 g) Fruit Juice: 3 oz (10 g) Chocolate milk: 1/3 cup (9 g) White milk: ¾ cup (10 g) Regular pop: 1/3 cup (9 g) Jam/jelly, maple syrup: 2–3 tsp (8–12 g) Skittles candy: 10–11 pieces (9–10 g) |
| More than 30 kg (66 lbs) | |
|---|---|
| Amount of carbohydrate required | 15 g |
| Fast-acting sugars and their carbohydrate content (g) |
Dextrose tablets: 4 (16 g) Fruit juice: ½ cup (15 g) Chocolate milk: ½ cup (15 g) White milk: 1–1¼ cup (12-15g) Regular pop: ½ cup (14 g) Jam/jelly, maple syrup: 1 tbsp (13 g) Skittles candy: 15 pieces (14 g) Honey: 1 tbsp (17 g) |
After your child has eaten the first dose of fast-acting sugar, wait 15 minutes then check your child’s blood sugar level again. If it is still low, give your child another appropriate dose of fast-acting sugar.
Wait for the sugar to take effect. This can be extremely hard. If your child is feeling hungry or dizzy, they might be tempted to eat and drink until the symptoms go away. However, this will result in a high blood sugar late in the day.
If the episode happens in the night or if your child will be participating in heavier than usual amounts of exercise, the second dose should be a high-glycemic index carbohydrate (sugar that will take longer to be digested and pass in the blood), such as:
- juice and a slice of whole grain bread
- milk and cereal
- yogurt plus fruit.
After the low blood sugar episode is resolved, it is important to try to determine its cause. If there is no apparent cause, then the insulin dose may need to be reduced.
Treatment of severe low blood sugar (hypoglycemic) events
If a mild low blood sugar (hypoglycemic) episode is not noticed or treated fast enough, symptoms can progress until they include:
- drunken-like behaviour
- very low energy
- loss of consciousness
- convulsions or seizures
- temporary paralysis.
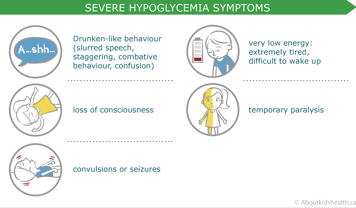
This is considered an emergency situation and your child will need immediate help. If they are unconscious or convulsing, they should not take fast-acting sugar by mouth, including liquids, because they are at risk for choking. Instead, they will need a glucagon injection.
Glucagon is a hormone that stimulates the liver to release sugar into the bloodstream. It is given by syringe and normally takes about 15 minutes to work. If you are too anxious to administer glucagon to your child, call 911 first and then attempt to follow the steps below:
For children who are suffering from extreme low blood sugar and who are unable to safely eat or drink:
- Confirm that the glucagon kit has not expired.
- Remove the lid from the glucagon.
- Remove the needle cap from the syringe.
- Inject the entire water contents of the syringe into the vial of glucagon.
- Remove the syringe from the vial.
- Swirl the bottle gently until glucagon has dissolved completely. The solution should look clear and look and feel like water. If the solution does not appear clear, do not administer the glucagon! Call 911.
- Insert the syringe in the vial and turn the vial upside down to withdraw the fluid. Make sure the needle tip remains in the solution.
- If the child is older than 5 years old, withdraw all the solution (1 mg)
- If the child is 5 years old or younger, withdraw half the solution (0.5 mg)
- Inject the glucagon as you would insulin, in the same spots.
After your child receives glucagon, check the blood sugar level and monitor your child. You should see a response in 15 minutes. If there is no response, call 911.
Once they are awake, offer sips of juice or other sugar-containing fluid. Once your child is drinking well, offer food containing carbohydrates.
If your child throws up after receiving glucagon, contact your diabetes team immediately.
All families of children with type 1 diabetes should have an emergency, usable (not expired) glucagon kit on hand and be comfortable using it.
Causes of mild low blood sugar (hypoglycemia)
Hypoglycemia is usually caused by one of three things: too much insulin, not enough food, or too much activity.
- Too much insulin: Mistakes happen. Sometimes a child will take the wrong type of insulin or the wrong amount at the wrong time.
- Not enough food: Sometimes your child will get caught up in an activity and forget to eat their snack, sleep through breakfast, or skip a meal.
- Too much unplanned activity: This is the most common cause of hypoglycemia. It usually occurs when children participate in a game of tag or soccer without advance preparation. Too much sugar is burned off, leaving an excess of insulin in the bloodstream.
Reducing the risk of mild low blood sugar (hypoglycemia)
Here are some things you can do to help prevent hypoglycemic episodes.
- Eat meals and snacks on time. A delay of even 30 minutes can cause hypoglycemia.
- Ensure the proper insulin dose is prepared and given. Younger children sometimes require close supervision.
- Plan for extra activities with prepared snacks or an insulin reduction; communicate with teachers and caregivers so you know when extra activities are taking place.
- If blood sugar levels are consistently low at the same time of day, work with your diabetes care team to lower the insulin dose.
- Equip your child with fast-acting sugar at school, and at home, make sure there is always fast-acting sugar nearby. Always have a glucagon kit at home, and make sure it is not expired and you know how to use it.
- Have your child wear a medical alert identification (such as a bracelet) or, if they are older, carry a wallet card.
What is "high blood sugar" (hyperglycemia)?
High blood sugar, or hyperglycemia, is defined as a blood sugar level of above 11 mmol/L.
High blood sugar levels are to be expected from time to time. Sometimes the causes are easy to spot: an extra piece of cake a birthday party, taking a blood sugar test too soon after a meal, or some insulin leaking out at the site of injection . Sometimes there is a less obvious reason, such as insulin that has been ruined by too much heat or cold. Sometimes there is no reason at all.
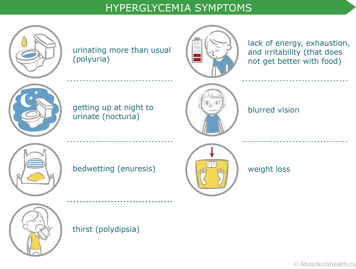
Hyperglycemia is concerning if it is combined with either ketones or blood in the urine or with any of the following symptoms:
High blood sugar symptoms
If a high blood sugar reading is combined with any of these symptoms, some additional rapid-acting insulin may be necessary. The diabetes care team can help assess whether rapid-acting insulin is needed, and will help you decide how much.
If hyperglycemia progresses without treatment, it can lead to a serious complication called diabetic ketoacidosis (DKA).