What is a medulloblastoma?
Medulloblastoma is the most common type of brain cancer in children. It belongs to a group of tumours called embryonal brain tumors. These tumors originate from immature brain cells.
Medulloblastoma arises from the cerebellum, which is located at the back of the brain. This part of the brain coordinates movement, balance, and posture and participates in some of the functions of the other parts of the brain in ways that are not fully understood. It is usually diagnosed in children four to eight years of age and is more common in boys.
Recently, scientists have been able to better understand the biology of medulloblastoma. They found that a medulloblastoma belongs to one of four subtypes called molecular subgroups, based on their genetic signatures. This helps doctors understand the different behaviours of a medulloblastoma, age of presentation and outcomes seen in children with medulloblastoma.
What are the symptoms of medulloblastoma?
Symptoms of medulloblastoma include:
- headaches
- vomiting
- unsteadiness (loss of balance)
- double or blurry vision
- neck pain or stiffness
- sleep difficulties
Children with this tumour may also have problems in school because tasks such as writing become more difficult. There may also be changes in their personality or behaviour.
Sometimes medulloblastomas block the flow of cerebrospinal fluid (CSF) through the pathways, or hollow channels, that drain CSF from the ventricles in the brain. This can lead to a condition called hydrocephalus.
Symptoms may not be obvious early on and may take time to become clearer. If the symptoms are dramatic, the diagnosis may happen quickly. If they are milder, it can take months. This is why some children are seen by a health-care provider after a few weeks of symptoms, while others with more mild symptoms can take a few months before they are seen. The diagnosis of any brain tumour can be a long and difficult process. However, your primary care team will be available to help guide you through every step.
What causes medulloblastoma?
It is not known what causes medulloblastoma. There is growing evidence that medulloblastoma is the result of a mistake that occurred in the early development of the brain’s cells. These cells will then grow uncontrollably to form what is called a tumor.
There is no way to predict that a child will develop a medulloblastoma and nobody is to blame if a child develops a tumour.
Researchers have been studying whether environmental factors, such as radiation, food, or chemicals, can cause brain cancer. At the moment, there is no definite proof that there is a connection.
Certain medical conditions are connected to medulloblastoma. If a child has Turcot syndrome or Gorlin syndrome, there is a slightly greater chance of developing a medulloblastoma. Your child’s primary care team will assess the need to do genetic testing. They may recommend a genetic test depending on the initial assessments and other tests, but this may not be needed for every child.
Medulloblastoma biology
Medulloblastoma is now divided into four subtypes called molecular subgroups, based on their genetic signatures. These groups differ in terms of their age of presentation, and behaviour. Researchers are still learning about the differences between these groups as there are still some unknowns, such as how these subgroups can be treated differently. The molecular subgroup testing is done on the tumor once it is removed, and results may take some time. Your primary care team will provide you with the results and explain what they mean.
How many children have medulloblastoma?
Medulloblastoma accounts for about 20% of all brain cancers in children.
In Canada, about 40 to 50 children are diagnosed with a medulloblastoma each year.
How is a medulloblastoma diagnosed?
Doctors and other health-care professionals will use well-established diagnostic tests to see if a brain tumour is causing your child’s symptoms. These tests will include a physical examination and brain scans such as magnetic resonance imaging (MRI) or computerized tomography (CT), which will identify the presence of a tumour. If medulloblastoma is suspected, you will meet with the neurosurgeons to discuss a plan for surgery.
A biopsy will be done at the time of surgery to confirm the diagnosis. During a biopsy, a sample of tissue from the tumour will be removed. This small piece of tumour will be sent to a doctor called a pathologist. They will look at the tumour under a microscope to learn the exact type of tumour.
The doctors may ask permission to study the sample tumour cells further to learn more about their biology. At the moment, the results of these tests do not influence treatment.
What is staging?
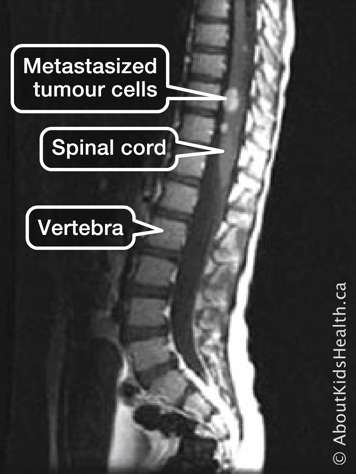
Staging determines if the tumor has metastasized (spread) to the spine or the CSF. To stage the tumour, the following diagnostic tools are used: CT scans, MRI of the brain and spine, and lumbar puncture.
To choose the type of treatment that is most appropriate, all the available information including the child’s age, staging and the biological characteristics of the tumor are used to match the best treatments to each tumor. Medulloblastomas are stratified into two groups, called "average risk" or "high risk", the group stratification determines the "intensity of the treatment" they will receive.
A medulloblastoma is called average risk if all of the following are true:
- All or most of the tumour was removed during surgery.
- The tumour cells have not spread to other parts of the brain or into the cerebrospinal fluid (CSF). This is seen from a lumbar puncture and MRI scan.
A medulloblastoma is called high risk if any of the following are true:
- Some of the tumour was not removed by surgery.
- The tumour cells have spread to other parts of the brain or into the CSF.
Before starting treatment, other tests such as blood tests and a hearing test are also done as a baseline to compare to during treatment.
How is medulloblastoma treated?
Once the health-care team has a clear understanding of what is causing your child’s symptoms — usually after surgery — a meeting with the team will be set up to talk about results and the treatment plan. Remember that it is helpful to bring paper and a pen or laptop to take notes at each meeting with this team. It is important to have the child’s primary caregivers in this meeting, for example both parents.
The treatment team may include a neurosurgeon, a neuro-oncologist, radiation oncologist, a nurse practitioner or nurse, and a social worker. During the meeting, they will explain which doctor is responsible for your child’s treatment, and the roles of everyone who is there. Other team members may be involved such as a dietician, pharmacists, occupational therapist, and physiotherapist, depending on your child’s needs. Every team member has their role in your child’s care, and everyone works together to make your child feel better.
The doctor will explain the type of tumour that your child has, based on what the team has learned through diagnostic testing. You will learn the expected effect this tumour will have on your child in the upcoming months and years, based on what is known about the tumour. This is called the prognosis.
The team may talk about placing your child on a protocol, which is a treatment plan for medulloblastoma. You will need to consent (agree) to the plan for the treatment to begin. Teenaged patients may be asked for their consent as well.
Your team will also talk to you about placing an IV line called a central line, this will help doctors give the treatments in a safer way and avoid multiple pokes for blood tests. You will get more information about the line insertion in details during the meeting.
There are three main modalities of treatment for medulloblastoma in children: surgery, radiation, and chemotherapy. For medulloblastoma, all three modalities are needed at different timelines to have the best results.
Surgery
Once a tumor is seen on the brain scans, the surgeons will assess your child for surgery. The surgeons will decide on the timing and approach for surgery. In some situations, the surgeons will need to relieve the pressure in the brain caused by hydrocephalus before the tumor removal surgery. This is done by placing a shunt to relieve the pressure.
To reduce some of the symptoms of the tumour and the swelling in the brain, your child will likely take steroids (an anti-inflammatory medication) to help reduce the swelling and improve the symptoms. This is usually done after the scans and around the time of surgery. Once your child is feeling better, the surgeons may stop the steroids.
Radiation therapy
Radiation therapy is high energy X-rays that kill tumor cells. You will meet with the radiation oncologist for a consultation to talk about how radiation therapy is given, side effects and how many treatment sessions are needed. This takes place after your child has had time to recover from surgery. In very young children, radiation therapy may be avoided due to the severe neurological side effects observed when given to the young developing brain. Your doctor will explain different therapies available to avoid or delay the use of radiation.
Chemotherapy
Chemotherapy is a type of medication that will kill cells that are dividing fast. This includes the tumor cells. Chemotherapy can be given by intravenous (IV) line or by mouth depending on what type of chemotherapy is needed. Your child’s neuro-oncologist and pharmacists will explain to you how and when chemotherapy is given. For children with medulloblastoma it is given after radiation therapy.
Clinical trials
Many doctors are trying to make cancer treatments more successful. They can do this by studying different types of treatment, in clinical trials. Your child’s doctor may ask if you would like your child to participate in a clinical trial. You will have to sign an informed consent form for your child to participate in a trial. The health-care team will explain the differences between being on a clinical trial and getting the standard treatment.
Additional supports
When you meet with the treatment team, you may also be told about resources available to support your child, you and your other children during treatment and recovery. You will be encouraged to think about any questions concerning the diagnosis and the treatment plan.
Before you agree to the treatment offered, it is important that you understand what to expect and feel comfortable with your decision.
What is the outcome for a child with a medulloblastoma?
The survival rate of children with medulloblastoma has improved significantly over the past 50 years. This was achieved using multimodal therapy, meaning the use of surgery and radiation followed by chemotherapy.
However, the outcome for a child with a medulloblastoma depends on many factors, including:
- the child’s age
- the biology of the tumor
- whether it has spread and by how much
- the type of treatment the child received
For medulloblastomas, the outcome is better if the child is in the "average risk" category. In general, the tumour is more likely to come back (recurrence) if the child is in the "high risk" category.
The risk of recurrence is higher during the first two years after diagnosis. However, recurrences can also happen later in life. This has been learnt over many years and after treating many children with medulloblastoma across the world.
Five years after treatment, 60% to 80% of children with medulloblastoma will survive. For children under the age of three, 20% to 50% will survive after five years.
There is increasing evidence to show that the biology of the tumour is essential to outcome. Doctors are trying to find out how to improve treatment for the different medulloblastoma subgroups while also reducing the late effects that can happen due to treatment.
It is important to keep in mind that every child is different. Speak to your child’s primary-care team if you have any questions about outcomes for your child.