What is an atrial septal defect (ASD)?
An atrial septal defect (ASD) is a hole or opening in the wall separating the two upper chambers (atria) of the heart. This wall is called the atrial septum.
In a normal heart, the right and the left side of the heart are separated. The right side of the heart pumps blood to the lungs to get oxygen. The left side of the heart pumps the blood high in oxygen to the body. To learn more about the normal heart, please visit the page "The normal heart".
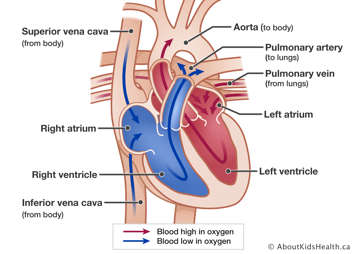
In an ASD, the hole between the atria allows blood to pass from the left atrium directly into the right atrium, then to the right ventricle and into the lungs. This extra blood flow to the right side of the heart can stretch the right atrium and the right ventricle.
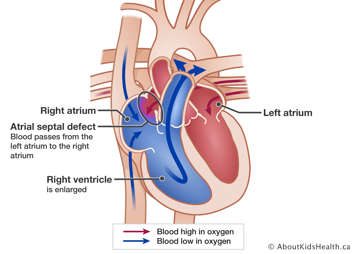
An ASD is present at birth (congenital) and can vary in size and location. There are different names for ASDs depending on where the opening is located within the atrial septum.
- Secundum ASD is located on the middle part of the atrial septum and is the most common type of ASD.
- Sinus venosus ASD is a rare type of ASD. It is located near the superior vena cava or inferior vena cava, the large veins that collect the blood from the brain and body. This type of ASD is associated with an abnormal connection of pulmonary veins to the right atrium instead of the left atrium.
- Coronary sinus ASD is extremely rare. It is located in the wall between the left atrium and the coronary sinus. The coronary sinus is a collection of veins which deliver blood low in oxygen to the right atrium from the heart muscle (myocardium).
How is an ASD diagnosed?
Most children with an ASD have no symptoms and will feel healthy.
An ASD is usually suspected when a doctor hears a heart murmur with their stethoscope. A heart murmur is the swooshing sound of blood flow through the heart, which can be either normal or abnormal. The murmur heard with an ASD is abnormal and is a result of extra blood flow to the lungs or blood flow through the ASD. An echocardiogram (echo) is performed to confirm the diagnosis. An electrocardiogram (ECG) and chest X-ray may also be performed.
How is an ASD treated?
In many cases, an ASD will close on its own before the age of two. If the hole is small and has not closed on its own, treatment may still not be needed. If the ASD is larger and the right side of the heart has become bigger, then it may require treatment. ASDs are normally closed with a procedure, in children aged 4-5 years and older.
There are two ways to close the ASD:
- Cardiac catheterization: During this procedure a thin, flexible tube called a catheter is inserted into a blood vessel in the groin that leads to the heart. The catheter is used to place a small device, called an occluder, over the ASD to close the hole. After a device closure of the ASD, blood thinning medication (acetylsalicylic acid – ASA) will be required for six months.
- Open-heart surgery: If closing the ASD with a device during a cardiac catheterization is not possible, surgery is needed. The surgery is performed using an incision in the middle of the chest (sternotomy) or through the ribs on the right side (thoracotomy). The ASD is closed using a patch. Sinus venosus or coronary sinus ASDs can only be repaired by a surgery, not a catheterization, and often even small ones need to be closed.
Both cardiac catheterization and open-heart surgery are very effective for closing of an ASD. When possible, cardiac catheterization is preferred, as the recovery time is much faster.
Does my child need to take antibiotic prophylaxis?
For 6 months following device or surgical patch closure of an ASD, antibiotics are recommended before routine dental work or certain surgical procedures to prevent infective endocarditis (an infection of the heart). When the heart tissue has healed over the closed ASD after 6 months, most children no longer require antibiotics.
What is the long-term outlook for children with ASD?
Children with a repaired ASD are expected to live as long as children with a normal heart. If the ASD was closed with a device, the device may affect nearby valves or vessels inside the heart. Although this is a rare occurrence, life-long follow up with a cardiologist is necessary. If the ASD was closed by surgery, complications are very rare, and life-long follow up may not be required.
Can patients with a repaired ASD exercise normally?
Regular exercise is important to keep both the heart and the mind healthy. In the past, children with congenital heart disease were often told not to exercise, or to not push too hard during exercise as the heart was weak. However, it is now known that for most children with congenital heart disease, regular exercise is beneficial to their overall health. All children with a repaired ASD should be physically active and can participate in all sports, even at a competitive level.
Children who have had a recent surgery should wait 3 months before returning to sports. Those who have had a catheterization should wait 1 month before returning to sports.
Pregnancy, sexual health and ASD
Pregnancy is considered safe for those with a repaired ASD or those with a small ASD that did not require treatment. Pregnancy increases the workload on the heart and for the majority of patients, this extra demand on the heart is well tolerated.
Every pregnancy has some risk for complications which can be increased by an underlying cardiac defect. It is important to speak with a cardiologist even before trying to get pregnant. In general, unplanned pregnancy should be avoided and seeking guidance from a cardiologist, family doctor or transition nurse about contraception choices is encouraged.
What method of contraception is recommended?
There are various contraceptive methods available for those with an ASD (see recommendations below). A doctor (e.g., your family physician, cardiologist, and/or gynecologist) or transition nurse can review options and provide guidance. Online resources such as www.iheartchange.org are also available. The Canadian Pediatric Society recommends long-acting reversible contraceptives (LARCs) as the preferred contraceptive of choice for all adolescents in Canada, as they are the most effective. LARCs in Canada are commonly called IUDs or intrauterine devices. LARCs or IUDs are safe for women with an ASD. IUDs have to be inserted by a doctor who is trained in the procedure and typically stay in the uterus for 3-5 years. Usually, this can be inserted by a doctor in the community.
Though the IUD is the most recommended form of contraception, alternative contraception options are also available. The combined oral contraceptive pill (‘the pill’) is generally safe.
Regardless of contraception choice, a condom should always be used to reduce the risk for sexually transmitted infections (STIs), and once sexually active, regular STI testing is recommended.
Emergency contraception such as 'the morning after pill' or 'Plan B' is safe for a person with an ASD who has had unprotected sexual intercourse.
Family history and congenital heart disease
The risk for any person having a baby with congenital heart disease is about 1%. For babies born into a family with a history of congenital heart disease, the chance that the baby will have any type of congenital heart disease ranges from about 2-10% depending on the type of heart defect.
Before becoming pregnant, a genetic specialist can provide information regarding family history and congenital heart disease. An ultrasound scan of the fetus’ heart can be performed during the pregnancy to look for congenital heart disease.