The main treatment to correct transposition of the great arteries (TGA) is the arterial switch procedure. This page explains what the surgery involves and minor risks of the procedure.
What is an arterial switch procedure?
Arterial switch is a surgical procedure and the main treatment to correct transposition of the great arteries (TGA). Almost all children with TGA undergo the arterial switch repair (also called the Jatene repair).
Soon after birth, babies with TGA become very sick because of a severe lack of oxygen. Before proceeding to an arterial switch, your baby’s condition can be improved by two temporary measures:
- starting a medication called prostaglandin
- doing a balloon atrial septostomy.
An arterial switch procedure is an open-heart surgery usually done within the first week of life.
Why is an arterial switch procedure done?
Without surgical correction, a newborn with TGA would suffer from lack of oxygen in the body and would not be able to live long. This procedure creates the pathways for a more normal circulation.
How is an arterial switch procedure done?
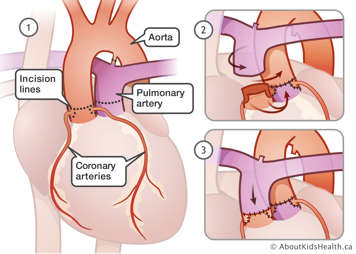
During the operation, the pulmonary artery and the aorta are "switched" so the blue and pink blood are flowing to their correct circulations. The coronary arteries are also surgically moved to their correct positions. The hole between the atria, which may have been enlarged by the balloon atrial septostomy, is also closed and the patent ductus arteriosus is tied off.
If your baby has a significant ventricular septal defect (a hole between the ventricles), the surgeon will close it during the procedure.
Risks of an arterial switch procedure
Although the arterial switch is a major surgical procedure, the results are excellent. More than ninety-nine percent of the surgeries are successful.
This operation will require the use of cardiopulmonary bypass (heart-lung machine).
Many children have minor complications such as:
- nausea
- feeding problems (such as trouble swallowing)
- bruising from intravenous (IV) sites. An IV line is a small tube that is put into a vein in your child's arm or leg to give medications or fluids.
Rare, serious complications of anesthesia and heart surgery include:
- bleeding, clotting, strokes
- vocal cord injury
- drug reactions
- heart rhythm problems
- cardiac arrest
- reactions to a blood transfusion
- brain injury
- breathing problems
Giving consent before arterial switch procedure
One of the doctors will explain the surgery and risks to you and answer any questions you may have about the procedure. When you are ready, you will be asked to sign the consent form for the operation.
Preparation for arterial switch procedure
Before your newborn’s surgery, you will meet with a number of health-care team members. The timing of these visits may vary but the team will check with you to make sure you understand what is happening and you have a chance to ask questions.
Pre-operative tests
Before surgery all newborns have:
- blood work
- an X-ray
- an echocardiogram
- an electrocardiogram
- an MRI imaging of the head (and sometimes an ultrasound).
All of these tests are done routinely to help the team prepare for surgery.
The surgical team
You will also meet the pediatric heart surgeon and the anesthesiologist.
The anesthesiologist will discuss general issues around having an anesthetic and specific issues about your child. These will include things like pre-operative sedation, blood transfusion and monitoring procedures during the surgery.
Blood transfusion
Most children who need heart surgery will need blood products during their surgery. This can involve transfusing:
- red blood cells to improve the amount of oxygen in the blood
- platelets to help blood clotting
- plasma
Food, drink and medication before the procedure
If your baby has been able to feed by mouth or through a tube, your nurse will make sure your baby stops feeding (fasting) at the right time before the surgery. The team will also make sure your baby gets the necessary medications and fluids through an IV.
On the day of the procedure
The anesthesiologist looking after your child will speak to you on the morning of surgery and answer any of your last-minute questions. The operating room nurse will also meet you and check your child. For safety reasons, parents usually do not come with children into the cardiac operating room for heart surgery. You will be asked to wait in a dedicated waiting room or another pre-set room.
During the procedure
Once your child is asleep, the team:
- puts in place IV lines and other catheters
- gives medications
- cleans the area where the incision (cut) will be madewith antiseptic (usually the sternum).
During this open-heart surgery, the anesthesiologist watches your child and the monitors, while communicating with other members of the surgery team, to make sure everything is stable.
Heparin (a blood thinner) is given because your child needs to be on a heart-lung machine. During this time, the heart is stopped while the surgeon repairs the defect. The perfusionist, the anesthesiologist and surgeon care for your child. They make sure that the heart-lung machine injects oxygen into the blood and is delivering the blood to the body and brain.
When the repair is complete, the heart is allowed to beat again and the heart-lung machine is turned down and off. If the heart is not quite functioning the way it should, medications are used to improve heart function.
An echocardiogram is done by the cardiologist to make sure that the repair is working the way it should. The surgeon then makes sure there is no bleeding and closes the incision.
Most heart surgery takes between three and six hours.
After the procedure
The anesthesiologist will transfer your child to the cardiac critical care unit (CCCU) when:
- the team is happy and confident that the repair is good
- heart function is good and stable
- your child is doing well on the ventilator
The care is then handed over to the team in that unit.
Recovery after the surgery
At hospital after the surgery
Your baby will likely spend a few days in the CCCU when recovering from their heart surgery. Your baby will then be transferred to the cardiac inpatient unit to finish their recovery.
The cardiac team:
- makes sure your baby's pain is managed with pain medication (most of the time acetaminophen; sometimes small doses of morphine as needed)
- looks after your newborn’s medications
- manages the tubes (drains) and wires that were placed in your baby’s chest during surgery
- takes care of the chest wound (sternal incision) and any other incision sites
- makes sure that your newborn is able to feed well
Before going home
Your baby is ready to go home when they are breathing comfortably and can feed well. During the recovery, the health-care team will teach you how to:
- look after the sternal incision
- give any medicines that your baby may need once at home
- take care of your baby (including giving a bath, changing diapers, feeding and holding your baby)
At discharge, you will be given a follow-up appointment for the first post-operative visit with a nurse practitioner. Your child will have regular follow-up visits with their pediatric cardiologist throughout childhood. Adults who have had an arterial switch operation for TGA in infancy will need lifelong follow-up with a cardiologist who specializes in the care of adults with congenital heart disease.